Basal Cell Carcinoma – Treatment in Israel
Most people associate skin cancer with melanoma – an extremely dangerous and aggressive tumor that forms from melanocytes, the skin cells responsible for synthesizing the dark pigment melanin. However, in 80% of cases, the skin is affected by a different, less aggressive form of cancer – basal cell carcinoma (BCC). This tumor develops from the basal layer cells of the epidermis, which are responsible for the constant renewal of our skin.
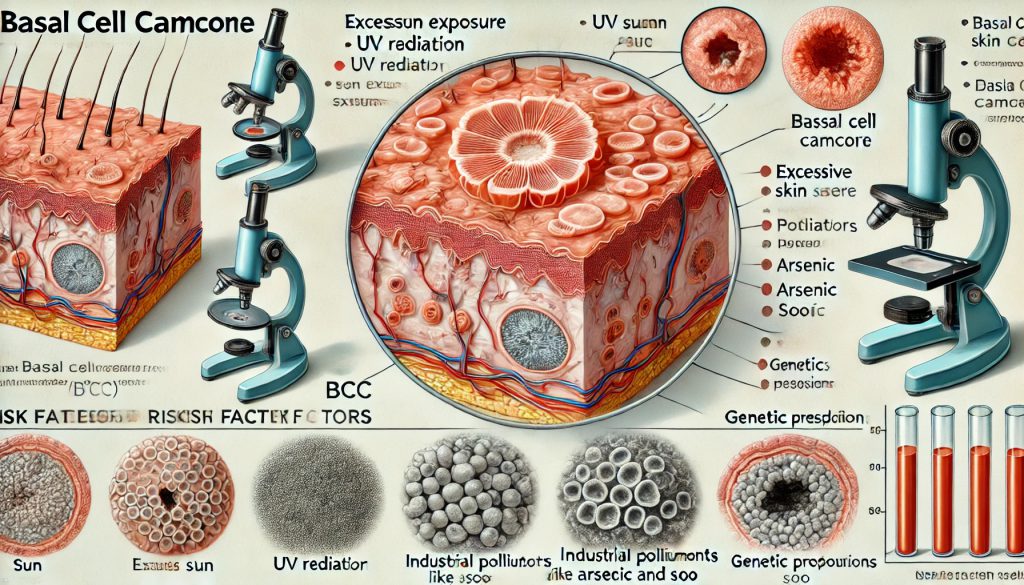
About the Disease
Basal cell carcinoma (BCC) – also known as basal cell cancer – is a malignant skin tumor that originates from atypical basal cells in the skin. Thanks to basal cells, the skin constantly renews itself, as new cells are formed to replace old ones when they die. BCC is classified as non-melanoma skin cancer, meaning it does not originate from melanocytes, the cells that produce melanin.
The basal (or germinal) layer is the lowest layer of the epidermis. Its structure includes specialized basal cells, which divide continuously. This is where the most common type of skin cancer originates.
According to ACS (American Cancer Society), over 5 million people in the U.S. are diagnosed with skin cancer annually, and 80% of these cases are basal cell carcinoma. In Russia, this form of cancer is diagnosed in more than 80,000 people each year, and the incidence rate is steadily increasing year after year.
Despite its high prevalence, the mortality rate for basal cell carcinoma is nearly zero.
Causes and Pathogenesis
The exact causes of basal cell carcinoma (BCC) are not yet fully understood. It is well established that benign cells transform into malignant ones due to genetic mutations. Various risk factors, both individually and in combination, have been identified and confirmed in research as contributing to BCC development. These include:
Prolonged Exposure to Ultraviolet (UV) Radiation
UV radiation physically damages the skin and directly affects DNA, stimulating mutations that can lead to the development of BCC. Prolonged sun exposure and frequent use of tanning beds significantly increase the risk of developing basal cell carcinoma. Artificial UV radiation from tanning lamps is just as harmful as natural sunlight.
Weakened Immune System
BCC often develops in patients who have undergone organ transplants or are receiving immunosuppressive therapy for other medical reasons. This type of therapy suppresses the body’s natural anti-cancer immunity, increasing the likelihood of tumor development.
Age Factor
Older individuals have a higher risk of developing BCC. This is because genetic mutations accumulate over time, partly due to cumulative exposure to UV radiation. According to the American Cancer Society, BCC most commonly occurs in patients over the age of 65, though it can also affect younger individuals.
Exposure to Chemical Carcinogens
Several harmful chemical substances have been linked to an increased risk of BCC, including:
- Petroleum hydrocarbons
- Coal tar
- Mineral oils
- Resins and arsenic compounds
- Insecticides and herbicides
- Other petroleum-based products
- Genetic Factors
A family history of cancer increases the risk of developing skin cancer, including BCC. If close relatives have been diagnosed with oncological diseases, the likelihood of developing BCC is significantly higher.
Unique (Individual) Risk Factors
Certain individual predispositions also increase susceptibility to BCC:
✔ Fair skin (Phototypes I and II) – Individuals with lighter skin tones are more sensitive to UV radiation and, therefore, more likely to develop BCC.
✔ Genetic Disorders – Some rare genetic conditions, such as xeroderma pigmentosum, dramatically increase skin sensitivity to UV radiation, making individuals highly susceptible to BCC.
Understanding these risk factors can help in preventing and detecting basal cell carcinoma at an early stage, allowing for timely medical intervention.
Symptoms of Basal Cell Carcinoma (BCC)
Basal cell carcinoma (BCC) typically develops in areas of the body not covered by clothing, such as the face, hands, and upper part of the head. Initially, a small, light pink or flesh-colored nodule or spot appears on the skin, resembling a mole, blemish, or thickened lump. This small, firm growth develops very slowly and does not cause any discomfort to the patient.
As it enlarges, the lesion may flatten, and the growth process is often accompanied by itching and bleeding. Many patients do not perceive these spots as dangerous, mistaking them for minor wounds or fatty deposits (lipomas).
BCC vs. Other Skin Cancers
One distinguishing feature of BCC compared to other types of skin cancer is that it has minimal tendency to metastasize—meaning it rarely forms secondary tumors in other parts of the body. However, it can grow extensively, penetrating deep into the skin and destroying adjacent tissues, cartilage, and even bone. When this occurs, severe pain may develop.
Key Symptoms of Basal Cell Carcinoma
The primary symptom of BCC is the appearance of an abnormal growth on the skin. However, BCC can manifest in different forms:
- Small, Translucent Nodules
- These tiny lumps are commonly found on the face and neck.
- They have a shiny or pearly surface and may develop visible blood vessels. If injured, they may bleed.
- Waxy Scar-Like Patches
- In some cases, BCC appears as white, waxy scars on the face and hands.
- The affected area is painless and resembles a slightly raised, waxy growth with no clear borders.
- The skin in and around the lesion appears tight and glossy.
- Open, Non-Healing Ulcers
- Slow-healing, open sores that persist for 2–3 weeks may be an early sign of BCC.
- These ulcers frequently bleed, form crusts, and reopen over time.
- If a wound remains persistently moist and does not heal, it should be evaluated by a doctor.
- Chronic inflammation with persistent wetness can be an early indicator of skin cancer.
- Localized Skin Darkening (Pigmented BCC)
- A recently developed dark bump that does not resemble a typical mole (nevus) may be a pigmented tumor.
- These growths vary in color, from brown to purple, sometimes with darkened zones.
- They typically have irregular, elevated edges.
- Burgundy or Red Spots
- These are one of the more common forms of BCC.
- Initially, they appear as small red dots, but over time, they expand and enlarge.
- These spots often develop in sun-exposed areas, such as the face, neck, arms, and shoulders.
- Without treatment, they can grow into large lesions.
- Pink Nodules with a Raised Edge
- These lesions have a raised, rounded border surrounding the affected area.
- Sometimes, a central crack or ulcer forms, covered with a dry blood crust.
- This is the most common presentation of BCC.
- These pink nodules often contain visible capillaries on their surface.
Additional Symptoms
✔ Persistent Itching – Many patients report itching in and around the affected area.
✔ Flaky or Peeling Skin – If there is no diagnosed allergy, but persistent, itchy, scaly patches are present, a dermatologist consultation is recommended.
✔ Progressive Growth – Over time, BCC lesions enlarge and change shape.
Most Common Locations for BCC
BCC does not appear in just one specific location but is more common in sun-exposed areas. It frequently occurs on:
- The face
- The scalp (especially in individuals with baldness)
- The neck
- The back
Because sun exposure is a major risk factor, areas not protected by clothing are at higher risk of developing BCC.
📌 If you notice any persistent or unusual skin growths, consult a dermatologist for an evaluation. Early diagnosis significantly improves treatment outcomes.
Types of Basal Cell Carcinoma (BCC)
Solid (Nodular) Basal Cell Carcinoma
This is considered the “classic” form of BCC, accounting for more than 75% of all cases. The tumor can vary in size (from a few millimeters to 5–6 cm) and may have a waxy appearance or be semi-translucent with red and blue vascular inclusions (“spider veins”). Nodular BCC grows slowly and is most commonly found on the face and neck, though it can occasionally appear on the body. If left untreated, it can penetrate deeper into tissues, affecting subcutaneous fat and even muscle structures, even if the external skin lesion remains small.
Ulcerative Basal Cell Carcinoma
This type initially develops as a nodular form, but over time, a small ulcer forms on its surface, sometimes covered with purulent crusts. In some cases, ulcerative BCC develops independently rather than from a nodular lesion. As it grows, tumor cells in the central part of the lesion break down, causing a progressive ulceration. The surface of the affected area becomes segmented, often featuring spider veins. Over time, the tumor’s growth leads to a necrotic or pus-covered ulcer, which represents an advanced stage of skin cancer.
Superficial Basal Cell Carcinoma
This type has low, smooth borders with a waxy coating, but lacks a distinct color pattern. Superficial BCC grows very slowly and can persist on the skin for decades. Its slow growth is due to its location, as it primarily appears on areas of the body that receive less sun exposure. This form is largely asymptomatic, meaning patients often do not notice it. Superficial BCC is more common in people under 40 and often resembles skin inflammation or psoriasis, presenting as reddish plaques with well-defined borders.
Flat (Sclerodermiform) Basal Cell Carcinoma
This is a rare but highly aggressive form of BCC. The tumor mainly develops on the skin of the head and neck, appearing as a dense, flesh-colored or light red patch with blurred edges. These lesions rarely bleed or ulcerate unless they become advanced. However, flat BCC can coexist with nodular BCC. Because of its appearance, it is often mistaken for psoriasis or eczema.
Fibroepithelial Basal Cell Carcinoma (Pinkus Tumor)
This is the rarest, benign form of BCC, clinically resembling nodular BCC. It typically appears on the body, most commonly on the lower back, and less frequently on the shoulders, thighs, or feet. Unlike other forms, it does not tend to bleed or ulcerate.
Pigmented Basal Cell Carcinoma
A variant of superficial BCC, this type contains both basal cells and melanocytes, giving it a dark brown or nearly black appearance, making it visually similar to melanoma. It is most common in people with Fitzpatrick skin types III and IV (darker skin tones).
Metatypical (Infiltrative) Basal Cell Carcinoma
Also known as basosquamous carcinoma, this type is a hybrid between basal cell carcinoma and squamous cell carcinoma, as it originates from keratinocytes (cells of the upper epithelial layer). Metatypical BCC is the most aggressive variant, capable of deep tissue invasion and metastasis to distant organs. Additionally, it has a high recurrence rate after treatment.
📌 Early diagnosis and treatment are essential for preventing complications and ensuring successful management of BCC. If you notice any unusual skin growths, consult a dermatologist immediately.
Stages of Basal Cell Carcinoma (BCC)
The development of basal cell carcinoma (BCC) is classified into the following stages:
Stage 0: The tumor is confined to the epidermis and does not invade deeper layers.
Stage I: The tumor has a diameter of up to 2 cm and may begin to invade the dermis (the middle layer of the skin).
Stage II: The tumor is larger than 2 cm in size.
Stage III: The tumor spreads to neighboring tissues, including muscles, bones, cartilage, and nearby lymph nodes.
Stage IV: The tumor metastasizes to distant organs.
Characteristics of BCC Growth
One of the key features of BCC is its slow progression. This allows for early detection, when the tumor is still highly treatable. Advanced-stage BCC is rare, occurring only when the tumor reaches large sizes (4–5 cm in diameter) and develops ulceration.
Late diagnosis is often due to patient neglect—individuals may ignore changes in their skin or fail to recognize the tumor’s presence. In older adults, cognitive impairments or limited access to medical care can also delay diagnosis and treatment.
Potential Complications of BCC
1. Recurrence
The most common complication of BCC is recurrence. Even after successful treatment, the tumor can regrow.
2. Increased Risk of Other Skin Cancers
Patients with a history of BCC have a higher risk of developing:
✔ Squamous cell carcinoma (SCC)
✔ Other types of skin cancer
Since squamous cell carcinoma metastasizes aggressively, untreated BCC can indirectly increase life-threatening risks.
3. Local Tissue Destruction
If BCC spreads, it can invade surrounding tissues, leading to:
✔ Cartilage and bone destruction
✔ Penetration into critical structures
If BCC reaches the brain, it can be fatal.
4. Lymphatic Blockage (Lymphedema)
In rare cases, if BCC is ignored for an extended period, it may invade deep soft tissues, blocking lymphatic circulation and leading to lymphedema (swelling due to lymph fluid retention).
📌 Early detection and timely treatment are crucial in preventing complications and ensuring a favorable prognosis for BCC. If you notice any suspicious skin growths, seek a dermatologist’s evaluation immediately.
Diagnosis of Basal Cell Carcinoma (BCC)
Basal cell carcinoma (BCC) is diagnosed and treated by an oncologist-dermatologist. The earlier BCC is detected and treated, the better the outcome!
How Is BCC Diagnosed?
Diagnosing BCC is relatively straightforward—a visual examination and patient history assessment (details about how and when the lesion appeared and changed over time) are often sufficient for an experienced dermatologist to suspect BCC.
If BCC is suspected, the first step in diagnosis is typically dermatoscopy. This is a highly informative, non-invasive diagnostic method that allows for early detection of malignant skin lesions.
During dermatoscopy:
✔ The doctor magnifies the suspicious area multiple times using a special optical device (similar to a magnifying glass).
✔ The dermatologist carefully examines all details of the lesion, including changes in shape, diameter, color, and contour.
✔ This method detects microscopic changes that may not be visible to the naked eye.
Tracking these progressive changes over time allows the doctor to select the most effective treatment approach and begin therapy immediately.
At On Clinic, qualified dermatologists and oncologists perform dermatoscopic examinations. Dermatologists use dermatoscopy daily and do not overlook critical changes in skin lesions.
Additional Diagnostic Tests
To confirm the diagnosis and assess overall health, the following tests may be recommended:
- Complete blood count (CBC)
- Blood biochemistry panel
- Urinalysis
- Palpation of regional lymph nodes to check for secondary tumors
Cytological and Histological Examination
The gold standard for BCC diagnosis is cytological and histological analysis.
✔ A tissue sample (scraping from the tumor’s surface) is collected.
✔ Cytological and histological tests provide 99% accuracy in diagnosing BCC.
Sentinel Lymph Node Biopsy for Metastasis Detection
If dermatoscopy or palpation of lymph nodes raises concerns about possible tumor metastasis, the doctor may order a sentinel lymph node biopsy.
✔ This method helps detect cancer cells in the sentinel (closest) lymph nodes—those that are first affected if the tumor spreads.
✔ While BCC rarely metastasizes, this test is crucial when tumor progression is suspected.
✔ Early detection of micrometastases enables prompt treatment intervention.
Imaging Studies for Advanced Cases
To rule out secondary tumors in the lungs, all patients undergo a chest X-ray before starting treatment.
If necessary, the doctor may also recommend:
✔ Computed tomography (CT) – For internal organ assessment
✔ Magnetic resonance imaging (MRI) – To detect metastases in the brain and spinal cord
📌 Early and precise diagnosis is key to effective treatment. If you notice suspicious skin changes, consult a dermatologist immediately!
Methods of Treating Basal Cell Carcinoma (BCC)
In the early stages of basal cell carcinoma, surgical removal is the primary treatment option. This involves complete excision of the tumor along with a small section of surrounding healthy skin to eliminate all cancerous cells and reduce the risk of recurrence.
Surgical Treatment Methods
1. Classic Excision with a Scalpel
✔ The surgeon removes the tumor along with surrounding tissue to ensure complete excision.
✔ The wound is then sutured, and the tumor fragments are sent for histological analysis.
✔ This method is less commonly used for tumors on the face or cosmetically sensitive areas, as it may leave noticeable scars.
2. Mohs Micrographic Surgery (Gold Standard for BCC Removal)
✔ This is the most precise method for removing BCC while preserving surrounding healthy tissue.
✔ The procedure is performed under local anesthesia and does not require hospitalization.
✔ The surgeon removes the tumor layer by layer, examining each layer under a microscope to ensure complete removal.
✔ The surgery stops once only healthy tissue remains, minimizing scarring and reducing unnecessary tissue removal.
✔ This method is especially effective for tumors on the face and other visible areas, providing excellent aesthetic results.
3. Laser Removal
✔ A non-invasive, bloodless technique that minimizes infection risks and complications.
✔ The laser beam cauterizes blood vessels, preventing bleeding.
✔ The depth of laser penetration can be precisely adjusted, ensuring that only cancerous cells are targeted while healthy tissues remain unaffected.
4. Curettage + Electrocoagulation
✔ The tumor is scraped away using a surgical curette.
✔ The wound is then cauterized (coagulated) with an electrical loop to destroy any remaining cancer cells.
✔ Healing occurs with minimal scarring.
5. Cryodestruction (Cryotherapy)
✔ This method destroys the tumor using extreme cold (liquid nitrogen).
✔ It is primarily used for early-stage BCC in cases where surgical removal is not an option.
Radiation Therapy
✔ Post-surgical radiation therapy is prescribed if regional lymph nodes were affected and removed during surgery.
✔ Radiation helps prevent recurrence and controls metastasis.
✔ Standalone radiation therapy is used when surgery is not an option (e.g., tumors near the eyes or delicate facial areas).
Chemotherapy for Metastatic BCC
✔ If BCC has metastasized, chemotherapy is recommended.
✔ The goal of chemotherapy is not to eliminate the tumor but to:
Extend the patient’s life
Reduce symptoms
Slow disease progression
Prognosis and Prevention
✔ BCC rarely metastasizes, so surgical removal is nearly 100% effective, especially if diagnosed early.
✔ There is no specific prevention method for BCC, but the most effective preventive strategy is UV protection.
How to Reduce Your Risk:
- Limit sun exposure, especially during peak hours.
- Use sunscreen with a high SPF (30+), reapplying every 2–3 hours when outdoors.
- Wear protective clothing and hats during high sun exposure.
- Avoid tanning beds.
✔ When working with chemicals or radiation sources, always wear protective gloves, jackets, and footwear to prevent chronic skin irritation or injury.
✔ Regular dermatological check-ups can help detect BCC at an early stage.
Why Choose Tel Aviv Medical Clinic for BCC Treatment?
✔ State-of-the-Art Equipment – We use premium-level medical technology that is safe for patients and convenient for specialists.
✔ Certified Clinical & Diagnostic Laboratory – Our European-standard laboratory ensures accurate and reliable test results, reducing waiting times and allowing for faster treatment.
✔ Multidisciplinary Approach – Our team of dermatologists, oncologists, and other specialists collaborate to develop a comprehensive and well-founded diagnosis and treatment strategy, minimizing the risk of medical errors.
✔ Globally Recognized Treatment Methods – We use proven, internationally accepted techniques to remove BCC without scarring and recurrence.
✔ Fast, Pain-Free, and Non-Hospitalized Treatment – Our procedures are performed quickly and efficiently, without the need for hospitalization, pain, or complications.
📌 Seek medical attention in time, and we will help you! Don’t delay your treatment—early detection is key!